MENOPAUSE
THERE IS A GREAT deal of confusion about menopause these days. I guess it’s better than the ignorance of years ago, but it’s still troublesome for the woman who’s trying to make sense of what this inevitable marker in her life will mean. Menopause used to be a virtual mystery; before the 1900s most women died around the age of fifty, a few years before the average onset of menopause. As Women lived longer, there were doctors who denied that menopause was anything but a psychological problem. Tranquilizers were thought to be the solution. Today, most women are familiar with the well-known symptoms of menopause: hot flashes, headaches, sleep disturbances, and changes in sexual function and desire. But there are other, long-term results of menopause that are the source of today’s controversy. At the heart of the controversy is whether menopause and its physical changes should be viewed as a natural event to be endured (or simply ignored by the many women who experience few symptoms), or whether it is an evolutionary mistake that can be corrected by the use of drugs.
Menopause, which usually occurs around the age of fifty, is, like puberty, a dramatic change in a woman’s body. At menopause, the ovaries, which have been releasing eggs since puberty, shut down and stop producing the hormone estrogen. (If a woman has had her ovaries removed surgically, she will experience menopause immediately due to the reduction in estrogen, no matter what her age.) Menopause does not happen overnight; for most women the process will play out over one to five years with gradually diminishing menstrual periods. During this time the amount of estrogen decreases, and it’s this decrease in estrogen that causes the typical symptoms of menopause.
The first sign of menopause for most women is irregular periods. The cycle may shorten or lengthen; the menstrual flow may increase or decrease. A woman can be fertile even if she’s been without a period for a year. After a woman experiences irregular periods for a year to five years, menstruation will stop. A year to a year and a half before a woman’s periods end, she may experience hot flashes, during which her temperature will rise and fall as much as 9 degrees. These flashes may be accompanied by sweating, heart palpitations, nausea, and, not surprisingly, anxiety. Hot flashes can contribute to insomnia; some women complain of waking frequently and having to change damp bedclothes. And some women also notice irritability, headaches, short-term memory loss, lack of sexual desire, and inability to concentrate. Some of these symptoms are not due to estrogen loss, but are simply a result of hot flashes and lack of adequate sleep.
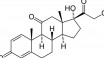
When you realize that more than three hundred types of tissues throughout the body have receptors for estrogen-which is to say that they’re affected in some way by the hormone-it’s not surprising that its decrease would cause physical changes. Estrogen affects the genital organs (vagina, vulva, and uterus), the urinary organs (bladder and urethra), breasts, skin, hair, mucous membranes, bones, heart and blood vessels, pelvic muscles, and the brain. It’s the loss of estrogen to these organs that causes the ultimate changes of menopause, including dry skin and hair, incontinence and susceptibility to urinary tract infections, vaginal dryness, and, most important, the diseases osteoporosis and heart disease. These diseases are at the center of the controversy concerning menopause: Because estrogen plays a role in preventing these diseases, should you replace the estrogen lost at the time of menopause with a synthetic version?
Before exploring this question, I just want to mention that not all women suffer the symptoms and diseases mentioned above. Many women sail through menopause with minimal discomfort. A few women never have a hot flash, some experience one or two hot flashes a month, and others have several an hour. Just as some women experience debilitating symptoms of PMS while others are symptom-free in relation to their menstrual cycle, so it is with menopause. Don’t expect to have symptoms; you may be one of the lucky ones who have none at all.
Estrogen replacement therapy, or ERT, and whether or not to take it, is an option that women facing menopause will have to consider carefully. You should not rely on anyone, including your doctor, to make this decision for you. There are too many variables that affect your best course of action, and you alone can decide. Here are some of the factors to consider:
BENEFITS
- Prevents osteoporosis
- Prevents heart attacks and strokes
- Prevents hot flashes
- Improves energy and mood
- Eliminates insomnia
- Prevents vaginal atrophy
- Prevents weakening of pelvic muscles
RISKS
- Possible increase of endometrial cancer
- Possible increased risk of breast cancer
- Blood dots or hypertension
- Gallstones
- PMS-type symptoms including breast pain and tenderness
- Frequent medical monitoring involving increased costs and potential for surgical procedures
Reviewing these benefits and risks will help you decide on the wisdom of ERT for you. For example, if you have a family history of breast cancer or endometrial cancer, these factors argue against ERT in your case. But a strong family history of osteoporosis might incline you toward ERT. All of the facts concerning your background should be weighed and discussed with your doctor.
Remember that the decision concerning ERT need not be forever. Some women take ERr for a year or two or three to get them through a highly symptomatic time of their menopause and then discontinue it.
Whatever you decide concerning ERT, there are natural means you can employ to minimize the discomforts of menopause.
Hot flashes are, for some women, the most troublesome symptom of menopause. They cause insomnia, resulting in irritability, and they can be uncomfortable and embarrassing. In my experience with my patients, drops in blood sugar can be the single most common precipitating cause of hot flashes; once the blood sugar is controlled, the incidence of hot flashes diminishes. In fact, by following the suggestions prescribed for Hypoglycemia, particularly eliminating sugar, reducing caffeine, eating meals at regular times, eating protein at lunch and dinner, and taking the supplement chromium, many women have told me that their hot flashes were dramatically relieved.
There are foods that can reduce menopausal symptoms. These foods, including soy flour, tofu, and other soy foods as well as linseed oil, contain substances called phyto-estrogens that can help compensate for the body’s loss of estrogen at menopause. Interestingly, in some societies, half of the dietary intake includes foods that contain phyto-estrogens; our typical diet contains less than 10 percent. In one study of healthy menopausal women who increased their intake of soy products or soy-containing foods for a period of six weeks, significant improvement was seen in the results of vaginal smears following the increased phyto-estrogen consumption.
The mineral boron has also proved helpful for my patients. Boron naturally elevates estrogen levels, and I originally recommended it to help fight osteoporosis. Many women told me that it had an immediate beneficial effect on their hot flashes.
Vitamin E has been helpful for many women who suffer from hot flashes, and sometimes when supplemented with vitamin C, it completely eliminates the symptom. Vitamin E is also useful because it decreases the tendency of blood platelets to clump together in menopausal women, which can contribute to heart attacks and strokes.
Many women complain of anxiety, irritability, and depression during menopause. As I’ve mentioned, these symptoms can be exacerbated by loss of sleep. Calcium supplementation generally has worked for all my patients, including menopausal patients, in helping them get to sleep and stay asleep. The mineral magnesium can also be helpful in relieving these symptoms.
Osteoporosis, which should be a concern for all women, becomes a pressing issue during menopause, when the estrogen supply diminishes and promotes increased bone loss. The most critical steps to take are to increase your calcium intake, in the form of foods and supplements, and to exercise.
Heart disease also becomes a threat. Prior to menopause, estrogen plays a protective role in relation to heart disease, but as estrogen production diminishes, the risk of heart disease increases. Ten years after menopause, a woman has nearly the same risk as a man of dying of heart disease. The major cause of this increased risk is a rise in the LDL (“bad”) cholesterol and a lowering of the protective HDL cholesterol resulting in vulnerability to atherosclerosis. In addition, the lack of estrogen causes the blood vessels to become less flexible, so blood clots can form more readily. Improved diet, exercise, and the use of supplements can all be helpful in preventing heart disease.
There is also an herb that can be helpful in relieving menopausal symptoms including hot flashes and depression. Dong quai (Angelica sinensis) has been proven to affect estrogen activity, and many women find it beneficial.
One of the most critical steps you can take to reduce the symptoms of menopause is to exercise. Countless studies have demonstrated that regular exercise can benefit menopausal women by fighting depression and anxiety, strengthening bone mass and lessening the risk of osteoporosis, reducing the risk of atherosclerosis, and improving one’s overall quality of life. I strongly recommend that all menopausal women adopt an exercise program.
Many women find that walking is a form of exercise that they can fit into their lifestyle easily and do on a year-round basis. There are a number of excellent books available on walking programs that will inspire you. Of course other forms of exercise such as swimming, aerobic classes, cycling, and dance are good choices, too. But exercise must be done regularly if it’s to be of benefit. I suggest that you exercise for a half hour five times a week.
One last note: In addition to the myriad problems associated with cigarettes, smoking encourages an early menopause. Women who smoke experience menopause four to five years earlier than women who do not smoke. Smoking also increases your risk of many of the symptoms of menopause, including osteoporosis and heart disease.
NATURAL PRESCRIPTION FOR MENOPAUSE
- Discuss the advisability of estrogen replacement therapy with your doctor. See text for a full discussion of this.
- Control blood-sugar levels in an effort to reduce hot flashes.
- Increase your Intake of soy-containing foods, including tofu and soy flour, as well as linseed oil (which is available in capsule form in health food stores) in the amount of 500 mg. three times daily.
- Reduce your risk of developing osteoporosis.
- Reduce your risk of heart disease.
- Adopt a program of regular exercise-at least 30 minutes, five times a week.
IN ADDITION TO YOUR DALLY SUPPLEMENTS, TAKE:
- Boron: 2 mg. daily.
- calcium: 1,200 mg. daily in the form of calcium citrate.
- Magnesium: 400 mg. dally.
- Vitamin E: 400 to 600 I.U. daily.
- Chromium: 100 mcg. three times daily.
- Dong quai, a Chinese herb available in health food stores. Take according to the package directions.