OSTEOARTHRITIS
WHAT IS OSTEOARTHRITIS?
Osteoarthritis is the most common type of arthritis, affecting an estimated 16 to 20 million adults in the United States. It is a slowly progressive disorder in which the cartilage that lines and cushions the joint gradually deteriorates. Eventually the bone underlying the cartilage is also weakened. New bone forms in abnormal locations at the margins and surface of the joint, often impairing joint function.
Osteoarthritis can be painful and very disabling, but it is not inevitably so. Often there is little or no pain and disability, even when joint damage is extensive. Good self-care can go a long way in easing symptoms and reducing reliance on pain medications.
WHAT ARE THE SYMPTOMS?
Pain associated with using a joint is often the earliest symptom of osteoarthritis. There may also be joint stiffness in the morning or after any long periods of inactivity. Usually this stiffness goes away within a few minutes when the joint is used. Pain can also be increased by prolonged joint use and can be relieved by rest. Gelling — a stiffness that is relieved by flexing the joint a few times — is particularly common with osteoarthritis of the hip or knee. Crepitus — a crackling or grating sound — may be noticed when the joint is moved.
Muscle spasms and reduction in joint motion can develop as the disease progresses. Bony growths (osteophytes) and loose bone fragments within the joint can also interfere with normal joint use. Flares — inflammation and a sudden worsening of pain — can occur if crystals form in the joint fluid (synovitis).
WHO GETS OSTEOARTHRITIS?
If you live long enough, you will likely have some degree of osteoarthritis. Roughly two-thirds of people in their 60s and 70s have osteoarthritis of the knee. Up to age 50, men are more prone to osteoarthritis than women, but after age 50, women are more likely to have osteoarthritis, often generalized arthritis affecting many different joints.
Osteoarthritis occurs most commonly in the hands, feet, knees, and hips, in that order. Multiple joint involvement is much more common in women, while osteoarthritis of hips, wrist, and spine is more frequent in men.
Generalized osteoarthritis, which includes bony enlargement of finger joints in addition to other joint involvement, tends to run in families. The enlarged joints so commonly seen in the hands of middle-aged or elderly women are called Heberden’s nodes.
Osteoarthritis increases with age because of changes in the bones and joints that occur with aging. Cartilage is 80 percent water and this water is lost with aging. Aging cartilage is more vulnerable to injury and less able to repair or rebuild after injury. The ligaments supporting joints are weakened so that the joint is less stable and more easily injured.
Severe injury to the joint or repetitive joint overuse are possible underlying factors in the development of osteoarthritis. In one study, osteoarthritis of the knee was more common in people whose occupations involved heavy labor. Some sports, such as soccer, appear to increase risk, at least at the professional or elite athlete levels. There is no evidence that recreational jogging increases risk, and good overall fitness is probably protective.
Population studies have revealed obesity to be the single most important risk factor and also the most preventable. Abnormalities in joints or bones present from birth, gout, diabetes, and hormonal disorders are other potential risk factors for the development of osteoarthritis.
HOW IS IT DIAGNOSED?
Diagnosis of osteoarthritis is based on clinical examination, supplemented by x-rays (radiographs) to assess the extent of joint damage. X-rays of affected joints will reveal joint space narrowing and the presence of bony growths (osteophytes) in the joint. These signs are generally considered to be the most reliable indicators of disease severity and progression. However, the joint damage shown on x-ray is not always linked to the severity of symptoms. Only 40 percent of people with severe osteoarthritis as seen on x-rays actually have significant discomfort and pain.
GENERAL TREATMENT ISSUES
Protect Joints: Good self-care generally involves protecting the painful joints, for example, using a cane or walker if necessary for severe osteoarthritis. For many people with osteoarthritis of the hip or knee, the most important step in protecting the joint is to lose weight. Weight increases the amount of force on a weight-bearing joint, which can accelerate cartilage breakdown. In one major study of osteoarthritis risk factors, a weight loss of roughly 11 pounds cut the risk of developing symptomatic knee osteoarthritis by 50 percent for women of average height.
Exercise: Protecting the joint doesn’t mean avoiding use of it. In fact, prolonged immobilization results in further deterioration of the joint cartilage. While sports or activities that stress or overuse the affected joints should be avoided, an appropriate exercise program consisting of fitness walking, swimming, bicycling, or other low-impact activities can be extremely helpful in improving muscle strength, mobility, and general well-being. Improving muscle strength may help to stabilize a joint and to distribute weight-bearing more evenly across the joint, again reducing the risk of further joint injury.
Exercise is important because older people with osteoarthritis tend to reduce their activity level, leading to loss of strength and mobility in other joints. For example, people with osteoarthritis of the knee commonly show a reduction in motion and strength in the ankle, which is rarely a site of osteoarthritis. Once ankle conditioning is reduced, the individual will begin to lose the strength and balance needed for normal walking, stair climbing, and getting up from a chair.
Apply heat and cold: Applications of either heat or cold can soothe aching or swollen joints. For swelling or pain due to inflammation, cold packs are more likely to help. Heat applications can be good for relieving joint stiffness. Otherwise, there is no clear advantage of one treatment over another, and the use of heat, cold, or alternating heat and cold is based on the individual’s preference. Cold can be applied in the form of cold packs or vapocoolant sprays, and hot packs, warm baths, and radiant heat all make good at-home heat treatments. Avoid applying hot or cold treatments to open wounds or sensitive areas of the body and do not leave the packs in place for more than 20 minutes. Some types of hot and cold packs should not be applied to bare skin, so follow directions in using these products to avoid tissue damage.
VITAMIN SUPPLEMENTS AND NUTRACEUTICALS
Vitamins: Some evidence suggests that optimal intake of the antioxidant vitamins A, C, D, and E may help treat or prevent osteoarthritis. Vitamin C is required for synthesis of collagen, a major component of cartilage. Vitamins D and A are both essential for healthy bones. Oxygen free radicals are believed to contribute to deterioration of cartilage in inflamed arthritic joints, so these antioxidant vitamins may have protective effects in slowing progression of the disease. Since the evidence supporting a role for vitamins and other antioxidants is based on laboratory studies and not clinical trials involving patients, significant proof that taking vitamin supplements will have an impact on osteoarthritis is lacking. However, a diet that emphasizes whole foods rich in these vitamins has multiple health benefits, including improved weight control. Good sources for these vitamins include:
Vitamin C: Citrus fruits and juices, strawberries, red bell peppers, broccoli
Vitamin D: Milk, eggs, liver, tuna, salmon
Vitamin A: Milk, eggs, liver, fish, carrots, broccoli, cantaloupe, tomatoes
Vitamin E: Nuts, vegetable oils, wheat germ, leafy greens
Nutriceuticals: Over the last few years, two “nutriceuticals,” glucosamine and chondroitin, both derived from animal products, have become extremely popular as treatments and even as “cures” for osteoarthritis. A number of small studies have documented good results with these two nutriceuticals, taken alone or in combination. However, most of these studies were sponsored by manufacturers of these nutriceuticals, and some experts express skepticism about the degree of improvement achievable with these products.
Glucosamine is a natural component found in most body tissues, including cartilage. Chondroitin is an extract prepared from the cartilage of cattle. Both glucosamine and chondroitin may take several weeks to produce any benefits. Taken orally as directed, these substances appear to be extremely safe. However, these nutriceuticals are often sold in combination formulas with other substances that have never been tested for safety. The most commonly used dosages are glucosamine 1500 mg and chondroitin sulfate 100 mg daily, for an average cost of $30-$45 per month. As with other herbal and nutraceutical preparations, some commercial brands of glucosamine or chondroitin have been found to contain much less of the active ingredients than claimed on the label.
Collagen hydrolysate (or hydrolized collagen) is another nutriceutical promoted for the treatment of osteoarthritis. It is basically a form of gelatin (a food) and therefore is very safe, but there is little scientific evidence indicating that it is effective. It is now being formally studied as a treatment for arthritis.
MEDICATIONS
The over-the-counter pain relievers available for short-term relief of arthritis pain are acetaminophen (Excedrin, Tylenol); aspirin (Bayer, Bufferin, Ecotrin); and the nonsteroidal anti-inflammatory drugs (NSAIDs), which include ibuprofen (Advil, Motrin, Nuprin), naproxen sodium (Aleve), and ketoprofen (Actron, Orudis). Despite the fact that they are available without prescription, none of these medications are risk-free if taken for prolonged periods of time. If taken for prolonged periods of time, aspirin and the conventional NSAIDs can cause ulcers or potentially severe gastrointestinal bleeding. Acetaminophen is generally considered the safest option for long-term use. The elderly, in particular, should consult their doctor about the proper dosage before taking any over-the-counter medication on a daily or near-daily basis.
Topical capsaicin cream is another over-the-counter option that appears to be both safe and effective. Capsaicin is derived from capsicum, the substance that puts the “heat” into hot peppers. It is applied to the skin over the joint two to four times per day. When first used, it produces a stinging or burning in the skin where applied, but this goes away with continued use.
Two important new arthritis drugs became available in 1999: celecoxib (Celebrex) and rofecoxib (Vioxx). These are the first of new class of nonsteroidal anti-inflammatory drugs, the COX-2 inhibitors, that have proved to be relatively free of gastrointestinal side effects (ulcers and gastric bleeding) compared to the older NSAIDs. While safer than conventional NSAIDs, the COX-2 inhibitors are equivalent in efficacy and are considerably more expensive.
In addition to prescription-strength NSAIDs and the new COX-2 inhibitors, the less addictive narcotic analgesics, such as codeine and propoxyphene (Darvon, Wygesic), have also been prescribed on a short-term basis for relief of osteoarthritis in combination with acetaminophen or other nonnarcotic pain-relievers. It is also sometimes helpful to supplement pain-relievers with tricyclic antidepressants. These drugs have analgesic effects of their own and can improve pain relief even for people who are free from depression or other mood disturbances.
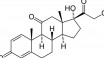
Corticosteroids and hyaluronate have both shown effectiveness when injected directly into the joint. Cortisone injections are useful for inflammation, but they can produce temporary synovitis or “flare” as a side effect. This flare usually resolves within a few hours and can be managed with cold compresses. Hyaluronate or hyaluronic acid derivatives injected into the joint are reported to reduce pain for extended periods of time (2-12 months) and to improve joint mobility.
SURGERY
Surgery can be considered to relieve intractable pain or to restore joint function. Good to excellent long-term results are reported for more than 90 percent of patients undergoing total hip or knee replacement.Osteotomy (surgery to remove part of the bone) may decrease stress on the joint and serve as an alternative to arthroplasty (reconstructive joint surgery). However, only half of patients with knee osteotomy maintain satisfactory results ten years after surgery. Surgical arthroscopy is useful for repair or partial removal of damaged knee cartilage. Surgical abrasion of cartilage can stimulate partial cartilage repair. Joint lavage (irrigating or washing out the joint) can be used with good short-term results to remove loose bone fragments or other debris in the joint space.
RESEARCH: THE DECADE OF THE BONE AND JOINT
The first decade of the new millennium has been declared the “Decade of the Bone and Joint” in recognition of both the disability caused by joint diseases such as osteoarthritis and the promise of ongoing research in relieving or preventing that disability. Objectives for the decade include:
Raising awareness of the growing burden of bone and joint disorders on society
Empowering patients to participate in decisions on their care
Promoting cost-effective prevention and treatment
Advancing understanding of bone and joint disorders through research to improve prevention and treatment
Current osteoarthritis treatments, ranging from aspirin to COX-2 inhibitors, generally only relieve symptoms and have little impact on the course of the disease itself. Newer treatments currently under investigation offer the potential of modifying the course of the disease and preventing or slowing its progression. Treatments now being investigated include:
Tetracycline derivatives that inhibit the enzymes that degrade cartilage
Pentosan polysulfate and other glycosaminoglycans
Growth factors (such as insulin-like growth factor I) and cytokines (such as TGF beta)
Avocado/soy nonsaponifiables (a derivative of the oils), which may enhance cartilage synthesis and repair